World Events Forum
Making the Best Even(t) Better
WE DO:
Meeting and event planning (including live webinars).
FOR HOW LONG?
We launched “our ship” to water in 2000.
FLAG:
“Make the best even(t) better.”
CREW RULES:
– perfectibility (not perfection)
– continuance (against permanence)
– the high art of interdependence (above independence)
– common sense
OUR SEXTANT:
We use it to measure the distance between two items: where is your event now? and where do you want it to be?, then propose a passage planning (voyage plan) from port departure to port arrival.
PASSAGE PLANNING:
We may correct the direction, suggest alternatives, warn of hurdles, provide potential outcomes but ultimately, your destination is yours, entirely. You lead, we design and build!
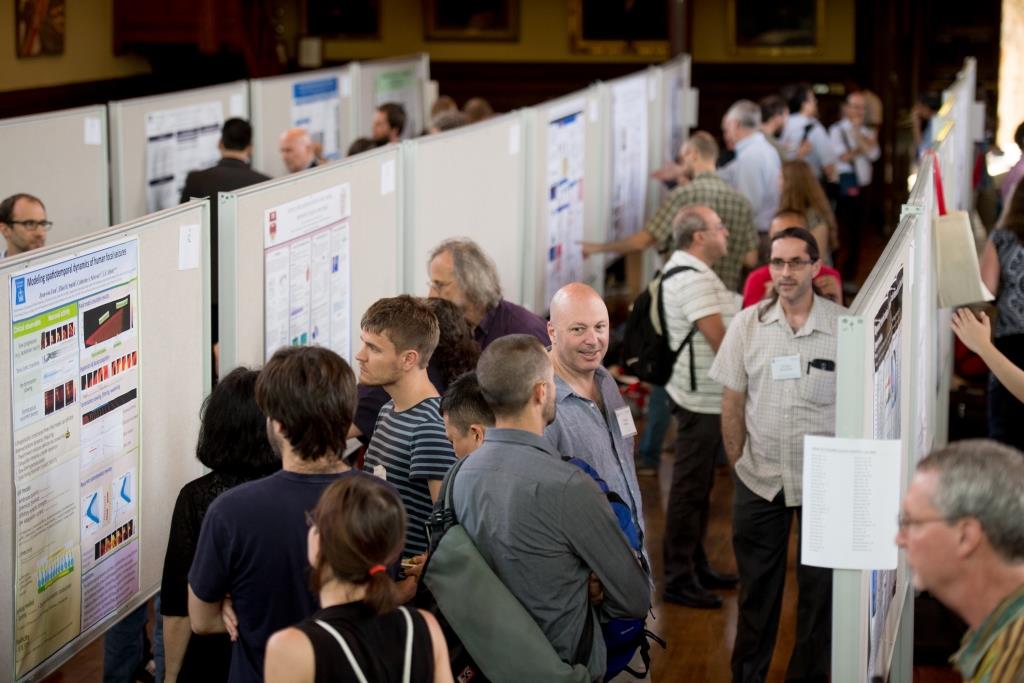
Meeting Planning Services
- Strategic planning
- Speaker management
- Location identification
- Venue/site selection and negotiation
- Event website creation and/or management
- Poster session, trade show and exhibit coordination/setup/management
- Registration (online/offline)
- Conference abstract intake/review (online)
- Conference syllabus (compilation, editing, publishing/printing) – online/print
- Liaison to client, registrants, sponsors, exhibitors, and vendors
- Meeting promotion/marketing
- Assistance with sponsorship solicitation
- Social/special event management
- Mobile app development and update
- Meeting logistics
- Financial recordkeeping & management
- Technical assistance
- Onsite administration, coordination and management
- Post conference administration
- Survey and evaluation
- Reporting

Special Events
- Support/Guidance in Identifying and Building Theme
- Site Identification, Selection, Contract Negotiation
- Vendor Selection/Contract Negotiation/Management
- Budget Development and Management
- Event Marketing (campaign development and deployment)
- Collateral Design (print and electronic)
- On-site Management
- VIP Arrangements
- Food and Beverage Selection/Coordination/Negotiation
- Audiovisual/Production Needs
- Registration Processing (online/print)
- Entertainment
- Silent/live Auctions
- Post-event Wrap Up/Audit

Association Management
MEMBERSHIP MANAGEMENT:
- Manage membership database and communications
- Provide secretariat services
- Processing membership applications and renewals
- Provide welcome-kits to new members
- Ensure compliance with association bylaws
- Manage membership renewal campaigns
- Report on membership status and assigned tasks/activity
VIRTUAL HEADQUARTERS:
- Serve as a virtual secretariat
- Maintain office, physical address, telephone and fax numbers for association
- Provide web and email addresses
- Forward voice and email messages to appropriate staff
- Maintain electronic and printed association files

Online Events/Live Webinars
- Provide overall planning and management of event
- Schedule the event with the various panelists and moderators
- Provide and present e-learning strategies and tools
- Provide technical assistance to attendees and panelists
- Provide training sessions for presenters and moderators
- Provide assistance with slide preparation and design
- Develop and deploy exit survey
- Develop exit testing/quizzes
- Compile and e-mail certificates of attendance

Assistance for medical tourists and foreign students
Hands-on concierge services consisting of, but not limited to:
- Schedule your medical appointments and helping with the preparation and submission of applications for educational programs.
- Meet-and-greet at the airport
- Arranging accommodation near your hospital or university at special rates.
- Catering to cultural preferences.
- Translation and interpretation services during your medical appointments.
- Assistance with the hospital paperwork and medication management.
- Help with social and cultural activities.
- Students, we’ve got your back with tutoring and academic guidance if you need it.
- Coordination of transportation.
- Hotline is available 24/7 with interpreters on hand.
Clients
2006 Torino Olympic Organizing Committee
Transfer of Knowledge
Alzheimer Research Forum
Webinars | Special Events | Exhibits
Alzheimer’s Disease: From Molecular Mechanisms to Drug Discovery Conferences
Website | Conference planning
Alzheimer’s Drug Discovery Foundation
Conference planning | Website | Mobile app | Virtual Conference
AlzPossible
Marketing and communications | Website | Webinars
American Aging Association
Marketing and communications | Website
Association of Corporate Counsel Indiana Chapter
Event planning

Brain and Behavior Research Foundation
Webinars
Break-In Club
Event planning | Marketing
Brown University
Website | Abstract Intake Platform | Event planning
Case Western Reserve University
Event planning
Columbia University
Event planning
CommonHealth Partners VA
Consulting | Website
FIFA (Federation Internationale de Football Association)
Consulting
Human Amyloid Imaging Conferences
Conference planning | Abstract intake/review processes | Website | Mobile app
Illinois Fatherhood Initiative
Event planning
IOS Press BV
Consulting
International Conferences on Alzheimer’s Disease and Related Disorders in the Middle East
Conference planning | Website
International Conferences on Molecular Neurodegeneration
Abstract Intake/Review | Conference planning | Website
Johns Hopkins University
Event planning
Kansas State University
Consulting
Laboratory of Neurogeriatrics, Case Western Reserve University
Website | Consulting
Lewy Body Dementia Association (LBDA)
Conference Website | Consulting | Event Planning
Longevity Project for a greater Richmond (LPgRVA)
Website | Consulting | Event Planning
Mount Sinai School of Medicine
Event planning
Mount Sinai Medical Center, Miami Beach
Conference planning | Website | Mobile App | Virtual Conference





Nordic Society of Human Genetics and Precision Medicine
Event planning | Consulting
Pharmaceutical Information Systems Association
Event planning | Administration
Pharmaceutical Research and Development Information Management Executive Forum
Event planning | Website | Mobile app
Pistoia Alliance
Event planning | Project Support
Prevent Alzheimer’s Disease 2020
Event planning
The Riverside Center for Excellence in Aging and Lifelong Health
Webinars
Schizophrenia Research Forum
Webinars | Tradeshow/Exhibit | Event planning
Special Olympics
Project management
United Arab Emirates Olympic Committee
Consulting and project management | Tradeshow/exhibit
United States Soccer Federation
Project management
University of Cincinnati
Conference planning | Website
University of the West Indies
Conference planning | Website
Virginia Commonwealth University, Department of Gerontology
Webinars | Website
Virginia Department for the Aging
Project management | Webinars
Virginia Department for the Aging and Rehabilitative Services
Webinars
Virginia Geriatric Mental Health Partnership
Webinars | Website
Voyager Pharmaceuticals
Conference planning
Walter Vlad Bolder Photography
And several other private clients


Locations where we have organized conferences:
United States
Arlington, VA
Atlanta, GA
Austin, TX
Bethesda, MD
Boston, MA
Bridgewater, NJ
Cambridge, MA
Charleston, SC
Chicago, IL
Cincinnati, OH
Cleveland, OH
Colorado Springs, CO
Deerfield, IL
Ft. Lauderdale, FL
Houston, TX
Indianapolis, IN
Jersey City, NJ
La Jolla, CA
Long Beach, CA
Los Angeles, CA
Miami, FL
New Orleans, LA
New York, NY
Philadelphia, PA
Plainsboro, NJ
Princeton, NJ
Providence, RI
San Diego, CA
San Francisco, CA
St. Petersburg, FL
Thousand Oaks, CA
Washington, DC
Rest of the Americas
Buenos Aires, Argentina
Cancun, Mexico
Montego Bay, Jamaica
Punta Cana, Dominican Republic
Toronto, Canada
Europe
Barcelona, Spain
Basel, Switzerland
Berlin, Germany
Bruxelles, Belgium
Bucharest, Romania
Budapest, Hungary
Gothenburg, Sweden
Lausanne, Switzerland
London, UK
Madrid, Spain
Manchester, UK
Milan, Italy
North Mymms, UK
Paris, France
Prague, Czech Republic
Seville, Spain
Sorrento, Italy
Stockholm, Sweden
Vienna, Austria
Zuerich, Switzerland
Asia
Abu Dhabi, UAE
Bangkok, Thailand
Dubai, UAE
Istanbul, Turkey
Lymassol, Cyprus
Male, Maldives
Singapore, Singapore
Tokyo, Japan
Selected 2023 Projects:
VCU Department of Gerontology Webinar and Online Training Series
Ongoing
vcugerontology
Brain & Behavior Research Foundation Meet the Scientist Webinar Series
Ongoing
bbrfoundation.org/events
Human Amyloid Imaging
Ongoing
hai.worldeventsforum.com/
ADDF's Investigator Day Conferences
PRISME Forum Spring and Fall 2023 Meetings
May and November
Gothenburg, Sweden and Boston, MA
prismeforum.org
PISA Annual Meetings 2023
March and November 2022
Barcelona, Spain and Online
MCI Symposium
March 2023
Online
mcisymposium.org
4th Workshop on Reserve and Resilience
December 2023
Bethesda, MD
reserveandresilience.com
Find us at:
1631 Whitcomb Ave
Des Plaines, IL 60018
USA
+1.224.938.9523
